Sacrospinous Ligament Suspension
|
A sacrospinous ligament suspension is a surgical procedure to restore the support of the top of the vagina, most commonly after hysterectomy.
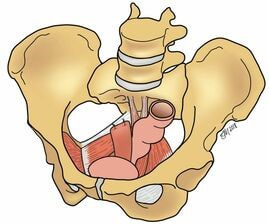
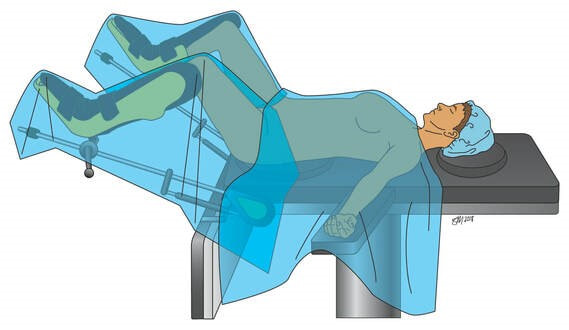
It can be performed at the same time as hysterectomy, or later on in life in women who have previously undergone a hysterectomy. In this surgery, the top of the vagina is sewn to the sacrospinous ligament, which is a strong, supportive structure that runs between the bones of the pelvis and the sacrum, thereby restoring its support. This type of prolapse procedure is referred to as a “native tissue repair” as we are utilizing your own tissue to restore the support of the vagina. How Is the Surgery Performed? At Northwestern Medicine, your urogynecologist will perform the sacrospinous ligament suspension through an incision in the vagina. Either permanent and/or slowly dissolving stitches are placed into the sacrospinous ligament and then through the top of the vagina; over time, scar tissue forms that supports the vagina. The surgery will be performed under general anesthesia with an anesthesiologist monitoring your heart and lung function throughout the surgery. Often, this surgery is performed at the same time as an incontinence surgery to treat urinary incontinence. How Successful Is the Surgery? This surgery has been extensively studied, and remains a good procedure for surgically managing the symptoms associated with vaginal or uterovaginal prolapse. Most women are satisfied with their symptom control following this surgery. Unfortunately, native tissue prolapse repairs do carry a risk of the development of recurrent prolapse. Approximately 30 percent of women undergoing this surgery will develop recurrent prolapse, which might prompt further conservative or surgical management options. Are There Complications? Given that this surgery has been extensively studied, the complications are very well known. As with any surgery, there is a risk of bleeding and hematoma formation following a sacrospinous ligament suspension. This is very rare and usually does not require a blood transfusion. There is also a small risk of vaginal or bladder infections after this procedure. If you develop a vaginal discharge that is foul-smelling or symptoms of a urinary tract infection (urgency, frequency, bladder pain, pain with urination), you should let your urogynecologist know. Specific risks unique to this surgery include buttock pain for the first few weeks after surgery; this happens to most women and can be treated with the pain medications you are given prior to your surgery. While rare, some women may develop pain or discomfort with intercourse; this can be treated with pelvic floor physical therapy. What Is the Recovery? Since your urogynecologist is able to perform this surgery through an incision in the vagina, you will most likely be able to go home the day of surgery. To help you accomplish this goal, we have worked with our anesthesiology team to develop an Enhanced Recovery After Surgery (ERAS) program. Your urogynecologist will determine if you are a candidate for this program at your pre-surgical visit. About Vaginal Surgeries Vaginal surgeries are minimally invasive procedures that require no incisions in the abdomen because access to all of the pelvic organs is obtained using incisions in the vagina. For these procedures, patients are positioned on their backs with legs and feet in supportive stirrups. Other vaginal surgeries include: |
To Request an Appointment
If you're suffering from a pelvic floor disorder, you don't have to live with the symptoms. To learn about treatment options, call 312.694.7337 to schedule an appointment with one of our urogynecologists. Other Vaginal Surgeries for Pelvic Organ Prolapse
MEET OUR TEAM
Our transdisciplinary team works together to ensure that each patient receives a tailored and highly individualized plan of care. |