Congenital Anomalies of the Bladder and Genital Tract
|
The genitourinary (GU) system includes:
We created a special clinic with Ann & Robert H. Lurie Children’s Hospital of Chicago to address these issues. The Collaborative Advanced Reconstructive Evaluation (CARE) Clinic strives to provide compassionate GU system care. The clinic’s care team includes:
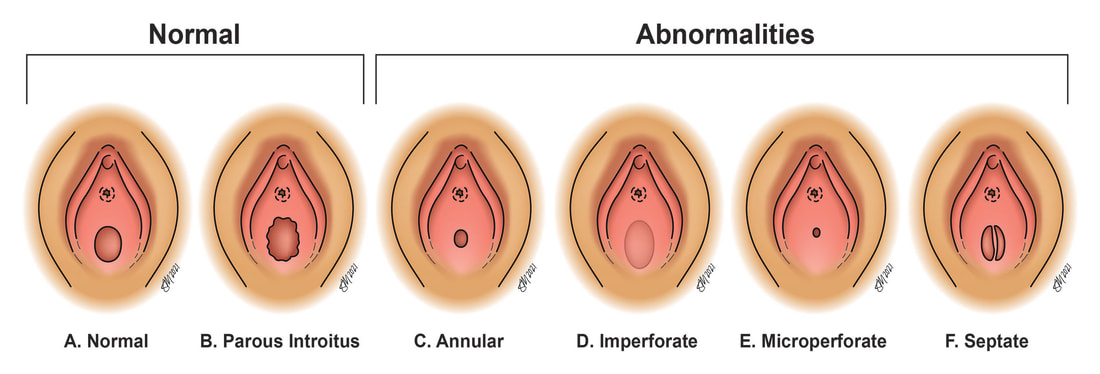
Congenital Anomalies of the Vagina/Hymen Anomalies of hymen The hymenal membrane consists of connective tissue attached to the vaginal wall. Variations can occur when there is loss of central degradation of the hymen during fetal development. This results in the presence of “excess” hymenal tissue that can block the opening of the vagina. This may make it impossible for menstrual blood to come out or for anything to go inside the vagina. Depending on the variation, the hymen can be completely imperforate (covering the entire opening to the vagina) or partially imperforate (only covering a portion of the vaginal opening). Anomalies of the vagina
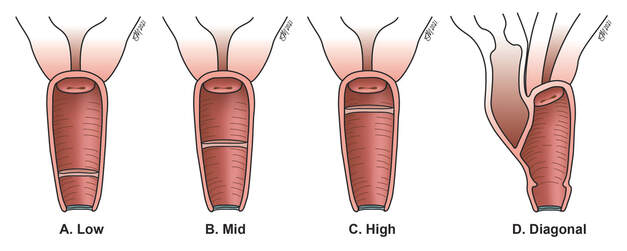
Septa are common vaginal anomalies in which there is extra tissue within the vaginal canal. Septa can be oriented either horizontally in the vagina (transverse vaginal septum) or vertically (longitudinal vaginal septum). These septa arise from different variations in the embryologic development of the vagina and can cause varying degrees of symptoms. They are each associated with different types of “co-variations” of development. Notably, transverse vaginal septa are associated with a higher risk of renal anomalies, and longitudinal septa are associated with uterine anomalies. Vaginal agenesis (absence of a vagina)
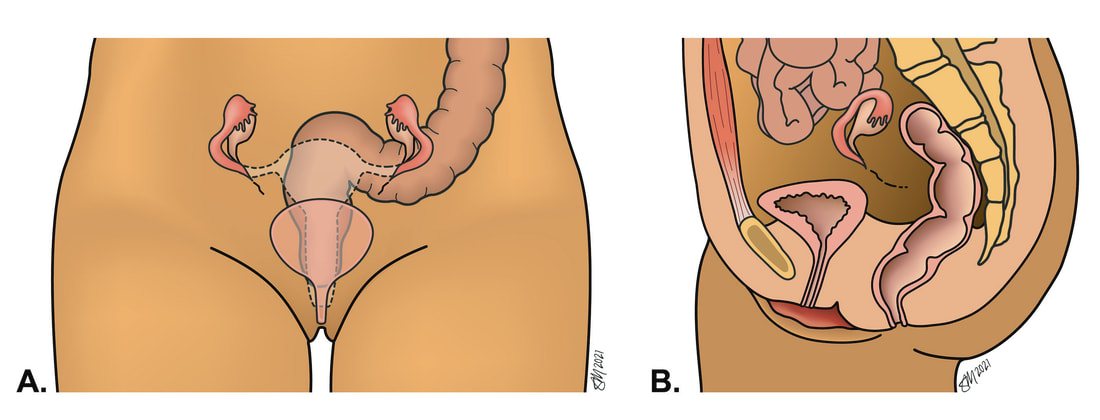
Absence of a vagina is a rare variation in development. Typically, girls are diagnosed in adolescence when they present to a doctor with the absence of a period. This is associated with various anomalies affecting the uterus, most commonly absence of a uterus. Notably, ovaries are typically normal with this type of variation. Anomalies of the uterus
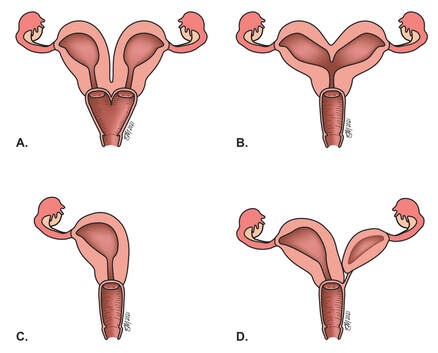
Defects involving the uterus are commonly referred to as Müllerian anomalies. They result from variations in the Müllerian tubes, the developmental precursors to the female reproductive structures as they exist at birth. The different types of uterine anomalies are often grouped with respect to their corresponding variation in the development of the Müllerian system. Common examples include didelphys uterus (image A), bicornuate uretus (image B), unicornuate uterus (image C), and arcuate uterus (image D). Congenital Anomalies of the Urinary Tract
Vesicoureteral reflux Vesicoureteral reflux is a condition in which the ureters are structurally abnormal and allow urine to travel backwards (toward the kidney), which is known as reflux. This can cause an increased risk of urinary tract infections and might require repair in childhood to prevent renal damage. Ectopic ureters Ectopic ureters refer to the abnormal orientation of the ureteral orifice (or opening). Sometimes the location of the orifice is within the bladder or urethra, or it can be located in the vagina. Duplicated ureters Complete or partial duplication of the urinary collecting system is the most common anomaly of the urinary tract, affecting 2–4 percent of the population. Bladder exstrophy Bladder exstrophy is a rare anomaly in which the bladder is exteriorized to the abdominal wall. The severity of this anomaly typically requires immediate surgical intervention in infancy. Women born with this anomaly often have normal reproductive potential but require a high level of supervision during pregnancy and delivery. Disorders of Sexual Development (DSD) Disorders of Sexual Development (DSD) are conditions in which the appearance of the external genitalia appear neither distinctly female nor male and are instead termed, “alternative” or “ambiguous.” Sometimes associated systemic manifestations are present which require immediate evaluation and intervention. However, slight variations in anatomy may not warrant evaluation until adolescence. The most common types of DSD are:
Causes The exact cause of congenital GU anomalies is not completely understood. However, we do know that most anomalies of the reproductive system occur during the 8th week of intrauterine growth and likely are due to the arrest of development of the preliminary structures. Some of the anomalies of the urinary tract and kidneys have been shown to be associated with diabetes in pregnancy. The development of the genitourinary system begins during the third week of embryonic growth and carries into the second trimester. The formation of the reproductive tract is closely associated with the development of the urinary system, which is why women with anomalies of the reproductive system commonly have anomalies of the renal system as well. How common are anomalies of the genital and urinary system? Anomalies of the genital system affect just over 5 percent of women. Congenital anomalies of the kidneys and urinary tract (CAKUT) are less common, affecting 4 in 1000 births. Symptoms Girls and women with GU anomalies that do not affect the external genitalia appear “normal” from the outside. These anomalies can be asymptomatic, causing few, if any symptoms, and typically are diagnosed later in life. However, some GU anomalies can cause symptoms in adolescence, including delayed periods, difficulty inserting a tampon, painful intercourse, or monthly abdominal pain. Some reproductive anomalies can cause difficulty later in the reproductive years during pregnancy and delivery, including miscarriage or preterm labor. While some types of urinary tract anomalies are asymptomatic, symptoms can include urinary tract infections. Other types of GU anomalies can be the manifestation of larger systemic syndromes, and symptoms are overt at birth, such as in Congenital Adrenal Hyperplasia (CAH). Treatments Managing symptoms directly related to anatomic variation Girls and women with symptomatic congenital GU anomalies typically have a variety of surgical and non-surgical treatment options. As each woman is unique, treatment plans are highly individualized to address her specific needs.
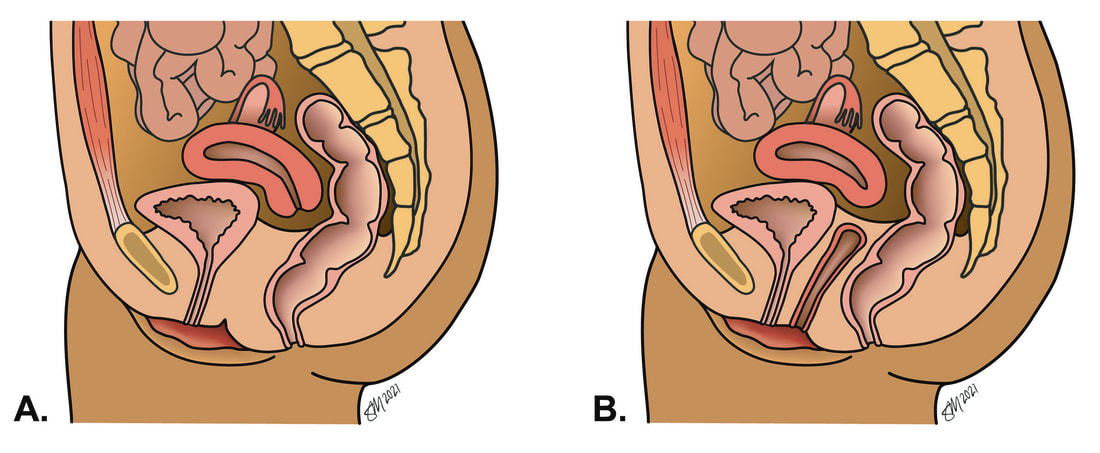
Managing reproductive outcomes in women with GU anomalies While variations of the urinary tract might not affect a woman’s reproductive potential, they might pose specific problems during pregnancy. In addition, women with a history of extensive surgeries for anomalies earlier in life are at risk for developing complications. These circumstances are best evaluated and treated with sub-specialty input from urogynecologic surgeons who are familiar with complex GU anomalies. Anticipating and managing reproductive and sexual health issues Women with congenital GU anomalies often can develop symptoms related to pelvic organ prolapse or urinary incontinence. While these symptoms usually can be managed with a variety of surgical and nonsurgical interventions, the presence of a congenital GU anomaly requires careful evaluation by a physician with experience treating this population. A woman’s sexual health also can be affected, and we offer a variety of treatment modalities to assist with improving her sexual function and satisfaction. |
To Request an Appointment
If you're suffering from a pelvic floor disorder, you don't have to live with the symptoms. To learn about treatment options, call 312.694.7337 to schedule an appointment with one of our urogynecologists. |