PELVIC ORGAN PROLAPSE
|
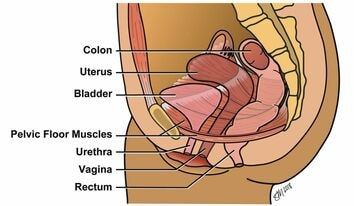
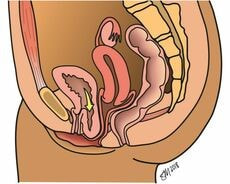
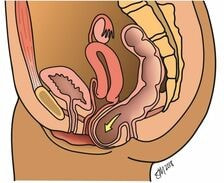
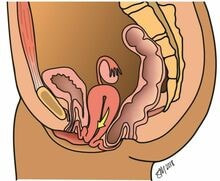
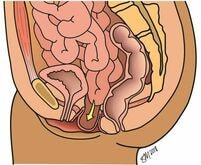
Pelvic organ prolapse occurs when the pelvic floor muscles and connective tissue weaken or tear, causing one or more of the organs inside the pelvis to slip from their normal positions and bulge into the vagina. The pelvic organs consist of the uterus, vagina, bowel, and bladder. Usually, the muscles and connective tissues in the pelvis support these organs and hold them in place.
Similar to a hernia, pelvic organ prolapse develops as soon as pelvic support fails but may not cause symptoms of a “bulge” until many years later.
As many as one in three women will develop prolapse in her lifetime, and close to 15 percent will have surgery. However, because there is a perceived stigma related to the symptoms of pelvic floor disorders, many women are reluctant to discuss them, even with their doctors, because of embarrassment. The urogynecologists at the Northwestern Medicine Women’s Integrated Pelvic Health Program (IPHP) perform comprehensive diagnostic evaluations and offer an array of appropriate treatment options for women with pelvic organ prolapse, and most women are candidates for both conservative and surgical options. The IPHP team is committed to providing individualized care for every patient. All surgeons are fellowship-trained and either board-certified or board-eligible specialists in the field of Urogynecology and Reconstructive Pelvic Surgery.
The Women’s IPHP is a national leader in pelvic organ prolapse treatment and research. Our transdisciplinary team works together to create new treatments and innovations to address each woman’s pelvic floor symptoms. Types of Pelvic Organ Prolapse
To evaluate a woman for pelvic organ prolapse, a urogynecologist will review her medical history and perform a pelvic examination, measuring the degree of prolapse. A staging system is applied to the exam findings, and a stage ranging from one to four is assigned. Below you will find descriptions of four types of pelvic organ prolapse, depending on the location of the support defect. It is possible, even likely, that a woman develops more than one type:
Symptoms
If a woman has pelvic organ prolapse, she may have one or more of the following symptoms:
If you have symptoms of pelvic organ prolapse, it is important that you consult with your primary care physician or obstetrician-gynecologist for a complete physical examination of the genitourinary and nervous systems. If other causes of your symptoms are ruled out, referral to a urogynecologist for further evaluation and treatment is appropriate. Causes and Diagnoses
There are several factors that may cause damage to the pelvic floor, including:
In addition to a thorough medical history and physical examination, your urogynecologist may perform some or all of the following supplementary tests:
Treatments
There are a variety of therapies, both surgical and non-surgical, that effectively treat pelvic organ prolapse and eliminate bothersome symptoms. Each patient is encouraged to consider her treatment goals and values and choose the treatment best suited to her. Options include: Active Monitoring Pelvic organ prolapse is not life-threatening, which means that if you do not experience discomfort, you may simply monitor its progress over time. It may stay the same size, or it could worsen as the years pass. Lifestyle Changes Some lifestyle changes can help reduce symptoms of pelvic organ prolapse, including:
Pelvic floor physical therapy helps rehabilitate the muscles of the core, which include the pelvic floor muscles, the abdominal muscles, the back muscles, and the diaphragm, and to optimize their function. Your physician will evaluate your pelvic floor muscles at your initial consultation and provide a referral if necessary. Learn about our Pelvic Health Physical Therapy Program. Pessary Therapy
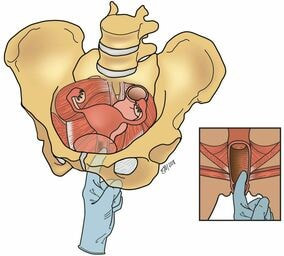
A pessary is a small device that is inserted into the vagina to mechanically support the pelvic organs above the pelvic floor muscles, eliminating the protrusion of tissue from the vagina. Pessaries carry minimal risk, as long as they are removed and cleaned regularly. Most patients can do this themselves, but those who cannot are seen in our office for pessary management by our advanced practice nurses. Women may choose this option if they have not completed their families, if they have medical problems that make surgery unacceptably risky, or if they personally wish to avoid surgery. Learn more about pessary therapy. Surgery for Pelvic Organ Prolapse Women desiring definitive treatment of pelvic organ prolapse may opt for a minimally invasive surgical repair. There are a few different surgical options, and a woman may benefit from one type of surgery more than another based on her age, prior surgical history, the severity of prolapse, overall health, and personal treatment goals. Your surgeon will help you determine which surgery is best for you. Pelvic prolapse surgery almost always involves repair of the vaginal apex, which is the uppermost portion of the vagina and includes the cervix or the vaginal cuff (in women who have undergone hysterectomy). Apical suspensions can be performed using one of three approaches:
In women who have not undergone hysterectomy, all three surgical procedures can be performed with removal of the uterus, fallopian tubes, and/or ovaries. Some women prefer to keep the uterus in place, and this can be offered in most cases. Women with pelvic organ prolapse often have urinary incontinence as well, and some are at risk of developing this problem after treatment for prolapse. For this reason, urinary testing is commonly performed before surgery for prolapse so that both problems can be treated at the time of surgery. Surgical Decision Making Because decisions about surgery for prolapse are complex and personal, it is important to understand that you are not alone. Our team offers a shared decision-making approach in which the ultimate choice of procedure is made during a discussion between you and your surgeon. During your consultation, you’ll receive an introduction to your surgical options and will be provided access to a computer-based module that provides educational materials and asks about your values and treatment goals. The results of your experience with this module serve as a starting point for your next discussion with your surgeon. This provides an ideal opportunity for all of your questions to be answered and for you to choose the best surgery for you. Recovery After Surgery Most women who undergo prolapse surgery will go home from the hospital on the day of surgery. Your physical activity will not be restricted, and you may return to your usual activities and exercise as soon as you feel up to it. Our team has published research showing that women who are able to resume physical activity as soon as they are ready have better surgical outcomes and quality of life than those whose activities are restricted after surgery. Learn more about the Northwestern Medicine Enhanced Recovery After Surgery (ERAS) program. |
To Request an Appointment
If you're suffering from a pelvic floor disorder, you don't have to live with the symptoms. To learn about treatment options, call 312.694.7337 to schedule an appointment with one of our urogynecologists. Treatment Options
Learn about common treatment options for pelvic organ prolapse: NORTHWESTERN MEDICINE ERAS PROGRAM
Our goal is to minimize negative outcomes of surgery, shorten recovery time, and help you get back to your life. |