Other non-Surgical Treatments
|
Non-surgical treatments often are sufficient in improving function and decreasing symptoms of pelvic floor conditions. The following are some of those treatment options:
Pelvic Floor Rehabilitation Pelvic muscle rehabilitation is often an essential part of treatment for pelvic floor disorders. Therapy includes pelvic exercises designed to train the pelvic floor muscles (known as Kegel exercises), which increases the patient’s ability to hold and release urine and stool. Many of these exercises can be done anywhere, at any time and in various positions, so they are easily integrated into everyday routines. In addition, pelvic pain disorders may be treated using pelvic floor muscle relaxation techniques and manual therapy. Targeting the right muscles is key with Kegels. Your doctor or physical therapist can help you determine how to most effectively contract your pelvic floor muscles. Many people find it difficult to contract and relax the pelvic floor muscles, so it's important for a healthcare provider to make sure that patients are doing the exercises correctly. The specialized physical therapists at Northwestern Medicine Women’s Integrated Pelvic Health Program are an excellent resource for this unique therapy. They use techniques such as biofeedback, electrical stimulation and manual therapy to optimize treatment and improve bladder and bowel function. Learn more about the Pelvic Floor Physical Therapy Program. Medication There are a variety of medications that treat incontinence. These medications are especially useful for treating an overactive bladder (OAB) associated with urge incontinence; however, many patients with mixed symptoms of OAB and stress incontinence will benefit from medical therapy. Some medications that may help with urinary incontinence include:
Some medicines that may be used to treat fecal incontinence include:
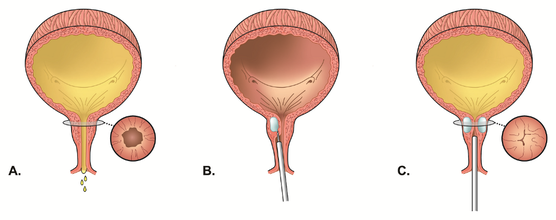
Pain disorders, such as painful bladder syndrome or pelvic pain, may be treated with neuromodulators, muscle/joint injections and other medications in conjunction with other treatments. Constipation can aggravate rectal prolapse and other defecation difficulties. Patients suffering from these disorders should avoid constipation. In some cases, dietary changes will be enough, but it's possible that medication may be necessary. All medications have the potential for side effects. Your healthcare provider will carefully weigh the risks versus the benefits of medications and will discuss all of the options with you before prescribing medication. Interventional Therapies There are a number of interventional therapies, including pessary therapy and Botox®, that can be used to help treat urinary incontinence, and these therapies are designed specifically for women. Another interventional therapy is bulking agents: Bulking agents Your doctor may inject very small, non-absorbable materials (image B) into the tissue surrounding the urethra to treat incontinence. This helps keep the urethra closed (image C) and reduces leakage of urine. Requiring minimal time and minimal anesthesia, this procedure can typically be done in your doctor’s office. Repeated injections may be required. |
To Request an Appointment
If you're suffering from a pelvic floor disorder, you don't have to live with the symptoms. To learn about treatment options, call 312.694.7337 to schedule an appointment with one of our urogynecologists. LISTEN NOW: OVERACTIVE BLADDER MEDICATIONS AND DEMENTIA
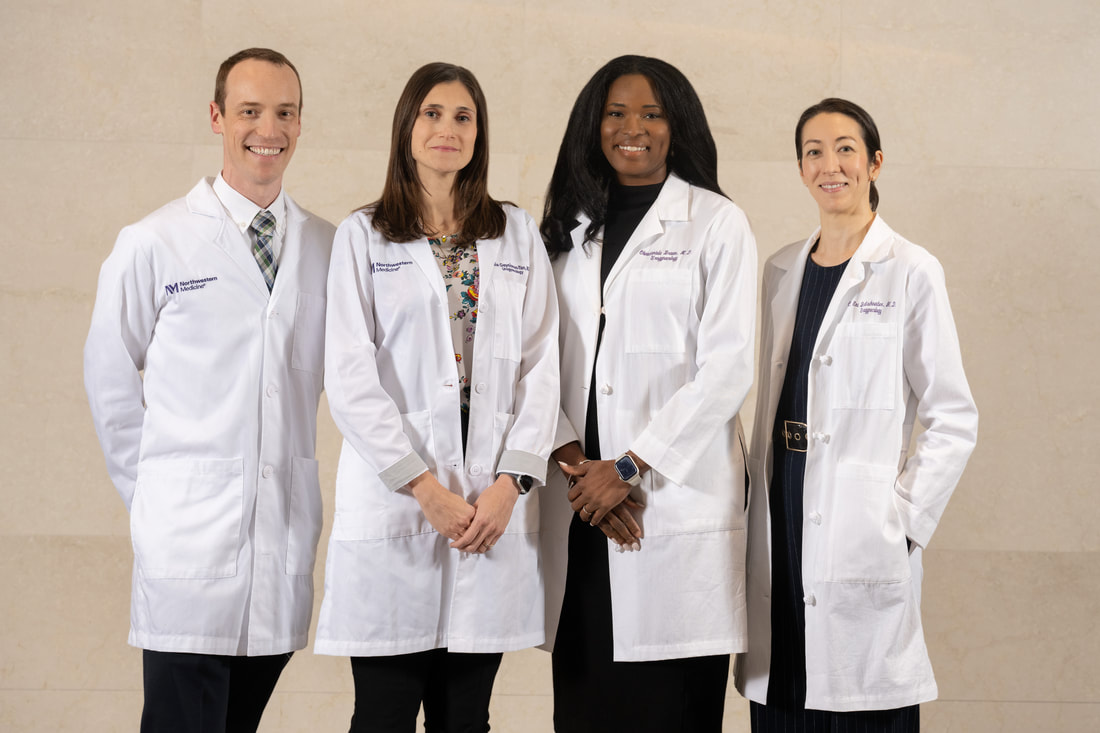
Dr. Emi Bretschneider discusses the link between dementia and medications used to treat overactive bladder. MEET OUR TEAM
Our transdisciplinary team works together to ensure that each patient receives a tailored and highly individualized plan of care. |