About Pelvic Floor Disorders
|
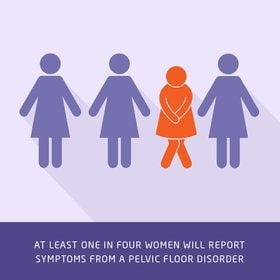
At least one in four women reports symptoms and a negative impact on her quality of life from a pelvic floor disorder, including pelvic organ prolapse, urinary tract symptoms or incontinence, and fecal incontinence.
Moreover, nearly one in five women will undergo surgery for a pelvic floor disorder with a 30 percent risk of needing repeat surgery. What Are Pelvic Floor Disorders?
Pelvic floor disorders are a group of conditions that affect the pelvic floor. The pelvic floor consists of the uterus, vagina, bowel, and bladder. Usually, the muscles and connective tissues in the pelvis support these organs to hold them in place. The pelvic floor prevents your organs from falling or protruding outside your body and plays an important role in how your organs work. When the pelvic floor muscles or connective tissue are torn or do not work properly, the pelvic organs may not function correctly and you may develop symptoms of a pelvic floor disorder. The three main types of pelvic floor disorders are:
While some risks for developing pelvic floor disorders can be mitigated by a healthy lifestyle, some risks are simply unavoidable. Aging is the most significant risk factor for developing a pelvic floor disorder, while childbirth is the second most important risk factor. With increased longevity, the prevalence of pelvic floor disorders among U.S. women is increasing dramatically. Treatment for women with these disorders is expected to increase by 40 percent over the next 40 years—from 28 million in 2010 to 43 million in 2050. About Urogynecology and Reconstructive Pelvic Surgery (URPS)
Recognizing the growing need for research and high-quality specialty care for women with pelvic floor disorders, The American Board of Medical Specialties (ABMS) officially approved the specialty of Urogynecology and Reconstructive Pelvic Surgery in the spring of 2011. In so doing, ABMS acknowledged that care for women with complex pelvic floor disorders (such as urinary and fecal incontinence, pelvic organ prolapse, and congenital abnormalities of the genitourinary tract) requires advanced fellowship training and board certification beyond the training acquired by a general obstetrician-gynecologist or a general urologist. In June of 2013, the American Boards of Obstetrics and Gynecology and Urology began certifying individual surgeons, and Northwestern Medicine is pleased to have an internationally renowned group of board-certified specialists in Urogynecology and Reconstructive Pelvic Surgery. Education We place a high priority on providing educational opportunities in an interactive and collaborative environment. We believe that it is critical to train the next generation of physicians to provide high-quality, patient-centered care for women with pelvic floor disorders for many generations to come. We are training academic leaders in Urogynecology and Reconstructive Pelvic Surgery, through our ACGME-accredited fellowship program. These future leaders will advance healthcare for women as surgeon–scientists who not only provide outstanding clinical and surgical care but also serve as inspiring mentors and educators. Clinical Programs The Northwestern Medicine urogynecology team offers an additional distinctive clinical program for particular groups of women with pelvic floor conditions.
|
To Request an Appointment
If you're suffering from a pelvic floor disorder, you don't have to live with the symptoms. To learn about treatment options, call 312.694.7337 to schedule an appointment with one of our urogynecologists. WHAT IS A UROGYNECOLOGIST
A urogynecologist is a fellowship-trained and subspecialty board-certified surgeon who specializes in the care of women with pelvic floor disorders. CONDITIONS WE TREAT
Learn more about pelvic floor disorders, such as anal incontinence, pelvic organ prolapse, and urinary incontinence. |